Bicornuate Uterus: Symptoms, Diagnosis, Treatment & Fertility Outcomes
Home | Bicornuate Uterus Treatment
As a fertility specialist, I understand that many women are diagnosed with a bicornuate uterus during fertility assessments and feel anxious about their chances of conceiving, carrying a pregnancy to term, or whether surgery is the only solution. Let me explain this condition step-by-step in a clear, simple, and evidence-based way.
What is a Bicornuate Uterus? (Definition)
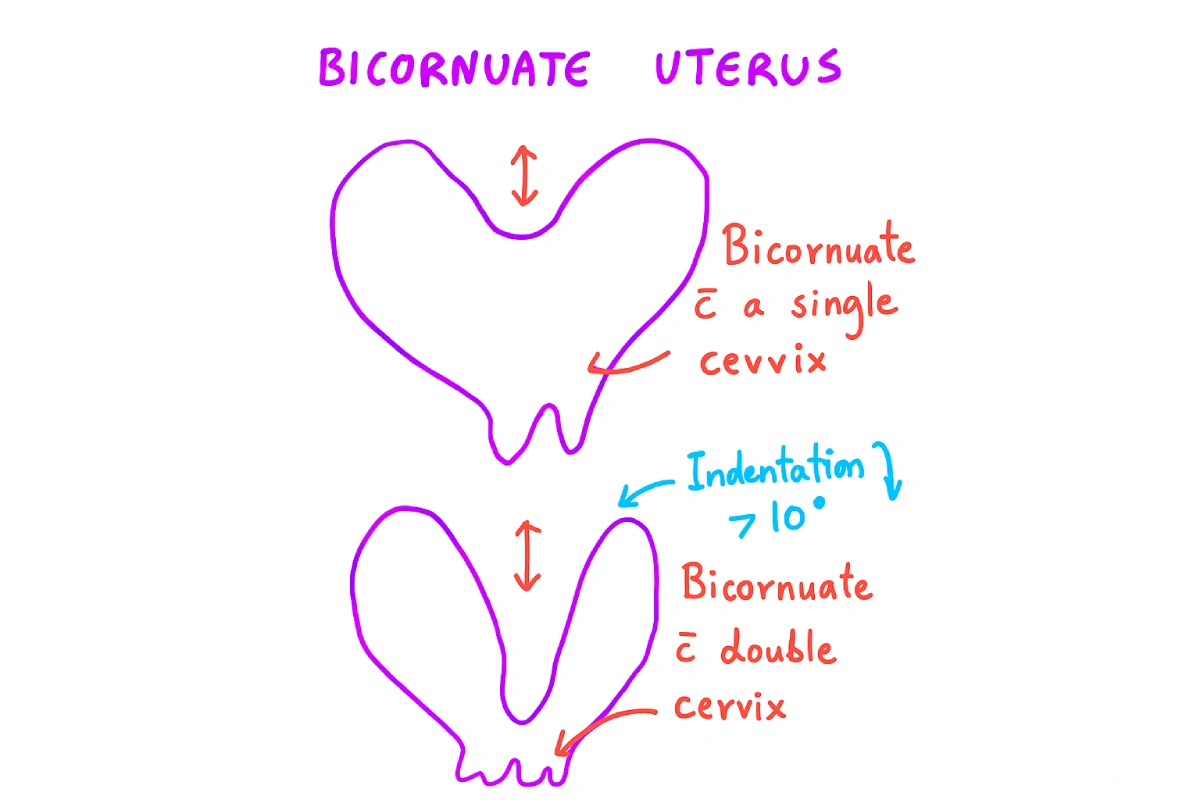
A bicornuate uterus—sometimes called a “heart-shaped womb”—happens when the top part of the uterus (the uterine horns) develops as two separate “horns” instead of one unified cavity. Imagine the uterus divided into two equal parts, which gives the uterus a distinctive indentation or dip at the top.
This isn’t something that just happens suddenly; it’s a congenital Müllerian anomaly, which means you’re born with it. The uterine structure develops this way during fetal growth due to incomplete fusion of the ducts that form the uterus.
What Causes a Bicornuate Uterus?
When it comes to the causes of a bicornuate uterus, the simplest answer is: we don’t know the exact reason for any individual.
Since a bicornuate uterus is a congenital Müllerian anomaly, it means the condition develops while a female baby is growing inside her mother’s womb. During this early developmental stage, two structures, known as the Müllerian ducts, are supposed to fuse completely to form one single uterus. In the case of a bicornuate uterus, this fusion is only partial, leaving the uterus divided.
There is absolutely no clue as to why it occurs to some and not to others. It is not caused by anything you did or didn’t do, nor is it linked to lifestyle, diet, or environmental factors. It is simply a developmental difference.

Get Expert Guidance from Dr. Jay Mehta—Müllerian Anomaly Specialist in India
What are the Symptoms of a Bicornuate Uterus?
This is a crucial point I emphasize to my patients:
In the vast majority of situations, a patient with a bicornuate uterus usually does not have any specific day-to-day complaint.
This structural difference rarely causes issues like pain or abnormal cycles in a non-pregnant state.
Remember one thing: The majority of the time, it is only diagnosed when the patient is either:
- Trying for fertility and undergoing an initial workup ultrasound.
- During an early pregnancy scan, the shape is noted.
- After experiencing recurrent pregnancy losses.
If you are not trying to conceive and are not having any issues, you may never know you have this condition.
How is a Bicornuate Uterus Diagnosed?
The most effective way to diagnose a bicornuate uterus is with a specialized 3-D pelvic ultrasound. MRI scans are also excellent alternatives for detailed images.
While performing these scans, doctors also check for any kidney or urinary tract abnormalities since these can be associated with uterine anomalies.
When viewed on ultrasound or MRI, you’ll see two uterine cavities, one on each side of the pelvis, separated by a clear division at the fundus.
The cervix may be single or occasionally double. The distinction between a bicornuate uterus and other uterine anomalies, like a septate uterus, is critical for appropriate management.
If you have been diagnosed with a bicornuate uterus and are worried about your fertility, know that expert care makes a huge difference. At Shree IVF Clinic, Dr. Jay Mehta specializes in managing complex uterine anomalies with advanced imaging and minimally invasive surgery.
👉 Book a consultation today at 1800-268-4000 and get clarity on your fertility journey with Dr. Jay Mehta.
Bicornuate Uterus Ultrasound & MRI Findings
The appearance is going to be absolutely standard; you will be able to see two cavities, both of them on each side of the pelvic wall, and both cavities will usually have an excellent endometrium inside.
It is also going to be important to note that the fundus is going to be divided. Many times, one may get to see a double cervix or a single cervix.
The findings of a bicornuate uterus on MRI are absolutely the same, just like how it is with the ultrasound.
What is the impact of a bicornuate uterus on fertility?
Many women are understandably worried about their ability to have a baby once they receive this diagnosis. The truth is that while a bicornuate uterus can affect reproductive outcomes, many women still carry successful pregnancies to term.
The core issue is one of space and volume.
In every case where there is a bicornuate uterus, the volume of the cavity can be reduced because the uterus is split into two horns. As a result, it can be one of the direct causes for:
- Primary Infertility: Difficulty conceiving in the first place.
- Recurrent Pregnancy Losses (Miscarriages): This is one of the commonest complications, as the embryo may implant in an area with restricted blood supply or limited space.
- Preterm Delivery/Preterm Labor: As the pregnancy progresses, the limited space can lead to a shorter cervical length or premature contractions, resulting in the baby being born early.
- Fetal Malpresentation: The limited space can cause the baby to settle into a position other than head-down (like breech or transverse), often necessitating a Cesarean delivery.
Bicornuate Uterus Treatment Options: Is Surgery Necessary?
In my practice, we follow an evidence-based, conservative approach.
For each and every anomaly that can be classified as a congenital Müllerian anomaly, the treatment of choice, where needed, is surgical correction. However, this is where the expertise comes in.
- Conservative Management (Observation)
The Majority Do Not Need Surgery.
If you have a bicornuate uterus but have not experienced any recurrent pregnancy losses (miscarriages) or preterm labor, you most likely do not require any form of surgical management. We simply monitor your pregnancy closely from the start.
- Surgical Correction (Strassman Metroplasty)
The surgical correction in this condition is only warranted in those patients who have had multiple, repeated abortions (miscarriages).
The goal is to unify the two separate horns into one larger, functional cavity.
- How We Decide: Usually, based on a 3D pelvis ultrasound, we can easily make a sound call as to which of the two uterine cavities is the healthier of the two.
- Unification Surgery: Very rarely, if both cavities are extremely small and recurrent loss is the primary issue, we can consider doing a unification of the bicornuate uterus (Strassman Metroplasty). This can be a great help to the patient.
- Complications to Consider: The outcomes of the surgical correction are also complicated by the risk of having a rupture of the uterus in a future pregnancy if the repair has not been done correctly. This is why this surgery is rare and should only be performed by a highly experienced fertility surgeon.
What is the difference between a bicornuate uterus and a septate uterus?
This is perhaps the most important point in the diagnosis and treatment plan. A septate uterus is often confused with a bicornuate uterus, but they are fundamentally different and have vastly different success rates after correction.
| Feature | Feature Bicornuate Uterus | Septate Uterus |
|---|---|---|
| External Shape (Fundus) | Heart-Shaped / Divided. The top of the uterus (fundus) is deeply indented externally. | Normal. The top of the uterus (fundus) is a single, smooth structure externally. |
| Internal Structure | Divided into two uterine cavities (two separate chambers/horns). | A wall (septum) of fibrous or muscular tissue divides the single cavity. |
| Surgical Correction | Strassman Metroplasty (Unification Surgery). More complex, typically open or laparoscopic surgery. Reserved for patients with repeated losses. | Hysteroscopic Septal Resection. Minimally invasive, relatively simple scope surgery. Highly successful. |
| Prognosis Post-Surgery | Improved, but can be complicated by uterine rupture. Surgery is rarely warranted. | Excellent. The volume of the cavity returns to almost normal, leading to great pregnancy outcomes. |
The glaring difference is that a septate uterus has an excellent, highly successful outcome once hysteroscopic correction is done for the septum. The bicornuate uterus is a more challenging repair and is reserved for specific cases.
What is the prognosis for a bicornuate uterus?
The most reassuring news I can give you is this:
The presence of a bicornuate uterus does not have any long-term health implications for the patient apart from affecting fertility and reproductive outcomes.
It does not increase your risk of cancer, chronic pain, or other major health problems later in life. Our focus is entirely on helping you achieve a successful pregnancy.
Key Takeaway
A bicornuate uterus is a congenital condition where the uterus is heart-shaped with two cavities.
Most women remain symptom-free and are diagnosed during fertility evaluations. It can increase the risk of miscarriage and preterm delivery, but not all cases need surgery. Surgery is reserved for women with recurrent pregnancy loss or poor fertility outcomes.
FAQs About Bicornuate Uterus Treatment
– Can a bicornuate uterus cause infertility?
Yes, it can sometimes lead to infertility, recurrent miscarriages, or preterm birth.
– Is a bicornuate uterus genetic?
A bicornuate uterus is a congenital anomaly (present at birth), but it is generally not considered a strongly hereditary or genetic condition that is passed down in families.
– Does every bicornuate uterus need surgery?
No. Surgery is only needed if there are repeated pregnancy losses or both cavities are very small.
– Is bicornuate uterus dangerous?
It is not dangerous for general health but can affect reproductive outcomes.
– How is bicornuate uterus different from septate uterus?
A bicornuate uterus has two cavities with a divided fundus, while a septate uterus has one fundus with a septum inside.
– Can I have a normal delivery with a bicornuate uterus?
Yes, a normal vaginal delivery is possible, but the risk of the baby being in a difficult position (like breech) is higher due to the irregular uterine shape. Your doctor will likely recommend a Cesarean section (C-section) if the baby is not head-down near term.
– Can women with a bicornuate uterus have a healthy baby?
Yes, many women with bicornuate uterus carry pregnancies successfully, sometimes with medical monitoring or surgical correction.
– How long is the recovery for bicornuate uterus surgery (metroplasty)?
Since the unification surgery (Strassman Metroplasty) is a major, often laparoscopic, abdominal procedure, the recovery is more substantial than for a septal resection. Typically, expect a few days in the hospital and a recovery period of 4 to 6 weeks before returning to full activity. You will also need to wait a recommended amount of time (often 6-12 months) before attempting pregnancy to allow the uterine wall to fully heal.
Dr Jay Mehta
Scientific Director & IVF Specialist with 10+ years of experience
CALL US 24/7 FOR ANY HELP
GET IN TOUCH ON


