WELCOME TO
Expert Care for Müllerian Anomalies: Restoring Hope & Fertility!
Müllerian anomalies like uterine septum, MRKH syndrome, bicornuate uterus, and vaginal agenesis can affect both health and fertility. With advanced diagnosis and corrective surgery, we help women overcome these challenges and achieve their dream of parenthood.
High Success Rates
10 + years of experience
ABOUT US
Helping you build the family of your dreams
At Shree IVF Clinic, we believe that every woman deserves a chance to experience the joy of motherhood—no matter how rare or complex her condition may seem.
For some, challenges like Müllerian anomalies—such as a septate, bicornuate, or unicornuate uterus—may make conception difficult or lead to pregnancy loss. But with the right care, compassion, and expertise, these obstacles can be overcome.
Led by Dr. Jay Mehta, one of India’s most trusted specialists in fertility and reproductive surgery, our team has helped countless women conceive after correcting these uterine anomalies—safely, naturally, and successfully.
At our clinic, you’re not just another case. You’re a story of strength, resilience, and hope waiting to be fulfilled.
SERVICES
Comprehensive Fertility Care and Services – Expert Solutions for Congenital Uterine Anomalies
As a specialized referral unit, we help women with the most complex reproductive tract abnormalities that can impact fertility and overall well-being. For those with a Müllerian anomaly, we aim for a precise, one-step correction to maximize the chances of a successful pregnancy.
Our fertility services support women and couples facing challenging reproductive issues.
We provide accurate diagnosis, advanced corrective surgeries, and fertility-preserving treatments, all delivered with compassionate, evidence-based care. By combining medical expertise, minimally invasive techniques, and personalized plans, we help you achieve your dream of becoming a parent.
What is a Mullerian anomaly?
A Müllerian anomaly is simply any form of developmental anomaly in the female reproductive system—this includes the uterus, fallopian tubes, cervix, and the upper part of the vagina.
During the development of a female embryo, there are two tube-like structures called the Müllerian ducts. These ducts must descend, fuse together in the middle, and then the central wall of tissue must dissolve (canalization) to create a single, clear uterine cavity.
The Cause: A Minor Developmental Hiccup
When there is a defective fusion or the canalization process is abnormal, it leads to the formation of a Müllerian anomaly. The cause is typically due to a differential canalization process—a simple abnormality in the duct’s developmental blueprint that happens very early in fetal life.
There’s no specific risk factor or something you did to cause this; it’s an event that occurs spontaneously, or sporadically, during development.
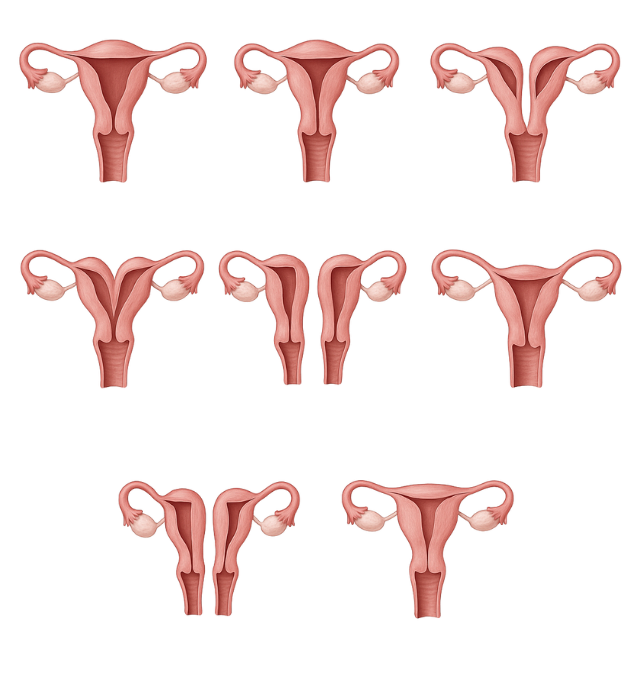
Categories /Types of Müllerian anomalies
Predominantly, the classification is simplified into two ways: obstructive and non-obstructive anomalies. Almost all the forms of obstruction that normally occur are also going to be associated with some of the other forms of severe pain in the abdomen, as well as endometriosis.
The majority of the time, it is the non-obstructive ones that are associated with no symptoms to start with and fertility once the patient ends up in the reproductive group.
MRKH Syndrome
MRKH syndrome is a congenital condition where the uterus and upper vagina are absent or underdeveloped. Surgical care can restore anatomy and fertility options.
Uterine Septum
A uterine septum is a wall of tissue dividing the uterus, often linked to infertility or miscarriage. Hysteroscopic surgery improves pregnancy outcomes.
Uterine Didelphys (Double Uterus)
A rare condition where a woman has two uteri, often with two cervixes. Surgery may be required if it causes infertility or complications.
Unicornuate Uterus
A unicornuate uterus forms from only one side of the uterus. It can increase miscarriage risk but pregnancy is possible with proper care.
T-shaped Uterus
A T-shaped uterus has a narrow cavity linked to infertility or miscarriage. Corrective surgery can restore normal shape and fertility.
OHVIRA Syndrome
OHVIRA combines a double uterus, blocked vagina, and missing kidney on one side. Early surgery restores anatomy and fertility.
Cervical Agenesis
Cervical agenesis is the absence of the cervix, causing obstruction and infertility. Advanced surgery can restore fertility potential.
Bicornuate Uterus
A bicornuate uterus has two cavities instead of one, sometimes affecting pregnancy. Surgery may be needed in cases of repeated loss.

Transverse Vaginal Septum
A wall of tissue blocks the vagina, causing pain and infertility. Surgery removes the obstruction and restores reproductive health

Mid Vaginal Atresia
In mid-vaginal atresia, part of the vaginal canal is missing. Surgery creates a functional passage and restores normal function.
What causes a Müllerian anomaly?
The exact cause is not fully understood. These anomalies arise when the Müllerian ducts do not develop, fuse, or canalize properly during embryonic development. This happens sporadically and is usually not linked to family history, genetics, or lifestyle factors.

Book Your Consultation Today with India’s Leading Müllerian Anomaly Specialist
– Dr Jay Mehta
Who can get a Müllerian anomaly?
There are no specific risk factors. These anomalies occur at birth and are considered congenital.
These conditions can affect any woman and are mostly sporadic. Most women are unaware of them until they either experience painful symptoms at puberty or struggle with fertility and pregnancy later in life.
Signs and Symptoms of a Müllerian anomaly
We simplify the classification of Müllerian anomalies into two main groups, which immediately tells us how and when they will affect a patient:
1. Obstructive Anomalies (The Painful Ones)
This category involves a blockage somewhere in the reproductive tract, which is why they are typically diagnosed very early in a girl’s life, usually within the first year of starting her menstrual periods.
Symptoms: They are predominantly associated with severe pain in the abdomen during periods (due to blood buildup that can’t flow out) and can lead to severe forms of endometriosis as the blood backs up into the pelvic cavity.
Examples: Transverse Vaginal Septum, some forms of cervical or vaginal atresia.
2. Non-Obstructive Anomalies (The Silent Ones)
These anomalies do not block the menstrual flow, so they are often associated with no symptoms to start off with. In fact, they usually go unnoticed until a woman begins trying to conceive.
Symptoms: They become problematic in the reproductive age group, presenting as infertility or recurrent miscarriages due to the abnormal shape or capacity of the uterus.
Examples: Septate Uterus, Bicornuate Uterus, Unicornuate Uterus, and Uterus Didelphys.
Do Müllerian anomalies affect fertility and pregnancy?
Yes, most Müllerian anomalies can impact fertility and pregnancy.
- A septum inside the uterus can increase the risk of miscarriage.
- Unicornuate uterus or didelphys uterus may lead to complications in pregnancy, such as preterm delivery.
- Obstructive anomalies can damage fertility by causing severe endometriosis.
Correcting the anomaly through timely surgery can dramatically improve fertility outcomes. That’s why it’s important to seek a specialist who regularly manages these cases.
What to Expect During Your First Visit?
The majority of the time, the patients who come to us as a referral unit have already been diagnosed.
However, we would undergo clinical examination as well as history taking in order to make sure that the urgency with which the surgery is going to be required is going to be classified and diagnosed for the patient.
Diagnosis: Imaging and Tests for Müllerian Anomalies
Since these anomalies involve the shape and structure of the internal reproductive organs, specialized imaging is necessary for a precise diagnosis.
1. Transvaginal or Transabdominal Ultrasound:
This is often the first step to visualize the general structure of the uterus and rule out other issues.
2. Magnetic Resonance Imaging (MRI):
In many situations, an MRI is the gold standard for pre-surgical evaluation, as it provides highly detailed, three-dimensional images.
This is vital for correctly distinguishing between anomalies like a septate uterus (which we can fix) and a bicornuate uterus (which we often don’t need to fix unless there are recurrent losses).
If you have been diagnosed with a Müllerian anomaly—or suspect one because of painful periods, repeated miscarriages, or fertility struggles—please don’t delay seeking expert care. With timely diagnosis and the right surgical correction, fertility outcomes can be greatly improved.
Book a consultation with Dr. Jay Mehta, a leading reproductive immunologist and Müllerian anomaly specialist in Mumbai, India, to discuss your options and create a personalized treatment plan.
Do all Müllerian anomalies need treatment?
This is a common and important question. The short answer is no, not all of them do, but the majority of anomalies that impact pregnancy will require corrective surgery.
- For instance, an arcuate uterus (mild indentation) generally doesn’t require surgery.
- A uterus didelphys (double uterus) often allows for successful pregnancy, though with a higher risk of preterm birth, and usually requires only monitoring, not surgical correction.
- The decision is based on a detailed discussion with us, taking into account the type of anomaly, your symptoms (pain), and most importantly, your future fertility concerns (recurrent miscarriage, infertility).
What is the best treatment for Müllerian anomalies?
The treatment discussion is always done based on the specific anomaly and the patient’s goal (relieving pain or achieving pregnancy).
- Septate Uterus Correction: This is the most common anomaly needing correction. We use a minimally invasive technique called Hysteroscopic Septum Resection (Metroplasty). This procedure is highly successful, dramatically improving the live birth rates for women with a history of miscarriages.
- Rudimentary Horn Excision: If you have a unicornuate uterus with a functional, non-communicating rudimentary horn, we must surgically remove that horn to prevent severe pain, endometriosis, and a high risk of uterine rupture during a potential pregnancy.
- Vaginoplasty/Septal Excision: For patients with obstructive anomalies like a vaginal septum or MRKH syndrome, the goal is often to create a functional vagina to allow for normal sexual intercourse (vaginoplasty) and relieve the painful blockages (septal resection).
Why choose Dr. Jay Mehta for Müllerian anomaly treatment in India?
At Shree IVF Clinic, Mumbai, we are nationally and internationally recognized as a leading referral unit for Müllerian anomaly treatment. Patients travel to us from across India and abroad for advanced surgical correction.
The biggest problem with the country of India is that patients often avoid traveling long distances for advanced medical care. Instead, they seek treatment at local hospitals or units that may not specialize in rare conditions like Müllerian anomalies.
Because of this, a large proportion of the cases referred to us are patients who have already had one or more surgeries performed without success.
As a referral center, we frequently manage these re-operated cases, which are often more complicated than primary surgeries. This highlights the importance of consulting a specialist from the very beginning for better outcomes.
Our approach focuses on:
-
Fertility-preserving techniques
-
High success rates in restoring normal fertility outcomes
-
Compassionate, patient-centered care
-
Expert surgeons experienced in complex corrections.
-
State-of-the-art imaging and surgical technology.
FAQs About Müllerian Anomalies
– Can Müllerian anomalies be detected early?
Yes, obstructive anomalies are often diagnosed during adolescence due to symptoms like severe pain. Non-obstructive anomalies may only be discovered later, during fertility evaluations.
– Are Müllerian anomalies hereditary?
Most cases are sporadic and not linked to family history.
– Can a Müllerian anomaly be prevented?
No. These are congenital (present from birth) and cannot be prevented.
– Does a Müllerian anomaly always cause infertility?
Not always. Some women may conceive naturally, but many require correction for successful pregnancy outcomes.
– Is surgery safe for Müllerian anomalies?
Yes. With an experienced reproductive surgeon, surgery is safe, minimally invasive, and improves fertility.
– Can Müllerian anomalies cause miscarriage?
Yes, especially a uterine septum or certain structural anomalies. Correction reduces this risk significantly.
– Can Müllerian anomalies be treated without surgery?
While some mild cases may not require intervention, most anomalies benefit from surgical correction to improve symptoms and fertility outcomes.
– How do Müllerian anomalies affect pregnancy?
They can increase the risk of miscarriage, preterm labor, and other complications. Early diagnosis and treatment are essential for a successful pregnancy.
– Why is specialist care important for Müllerian anomalies?
Specialists have the expertise and technology to accurately diagnose and treat these complex conditions, ensuring the best outcomes.
– Can I still get pregnant naturally after Müllerian anomaly surgery?
Yes, absolutely. The primary goal of corrective surgery, especially for a septate uterus, is to restore the normal uterine cavity, which can dramatically increase live birth rates (studies show success can jump from less than 10% to over 80% after resection). For anomalies that don’t need surgery (like some didelphys uteri), natural pregnancy is also possible, though you’ll need specialized monitoring due to a higher risk of preterm birth.
– What long-term follow-up is needed after the corrective surgery?
For most procedures, like hysteroscopic septal resection, the follow-up is minimal and involves ensuring the uterus heals correctly. For corrective surgeries like vaginoplasty (for MRKH), ongoing care, including vaginal dilation, is essential for long-term functional success. We tailor the follow-up to your specific procedure.









