MRKH Syndrome: Causes, Symptoms, Diagnosis, and Treatment
Home | MRKH Syndrome Treatment
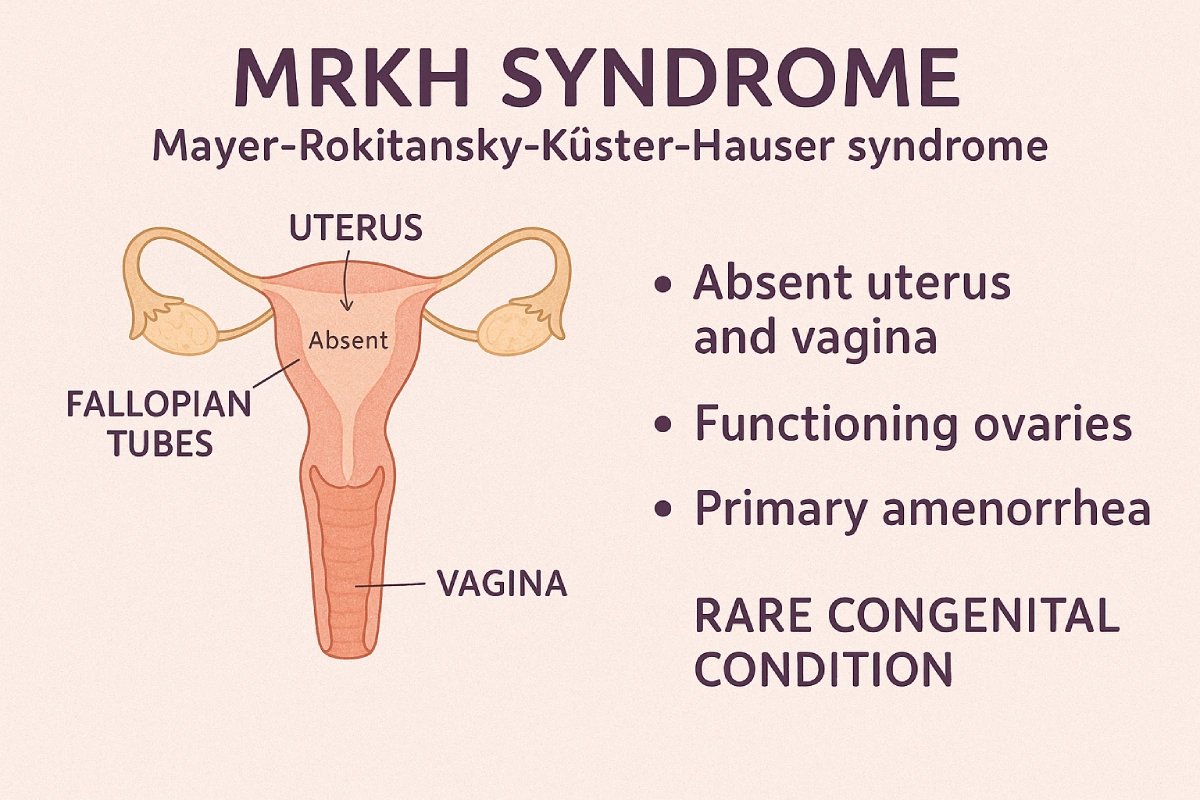
Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome is a congenital condition affecting the development of the female reproductive system.
As a gynecologist and fertility expert, I’ve seen how this condition can deeply impact a woman’s physical and emotional well-being. Here, I’ll explain MRKH syndrome step by step—what it is, the reasons it develops, how it’s diagnosed, and the treatment choices.
What is MRKH Syndrome?
MRKH stands for Mayer-Rokitansky-Küster-Hauser syndrome. It is a congenital anomaly of the vagina, where there is a developmental issue. Due to this, there is an abnormal formation of the vagina, and it is typically associated with an absent vagina in the majority of patients.
MRKH is associated with a varying degree of abnormalities; it could be associated with:
- Partial or complete absence of the uterus
- The majority of the patients only have the lower 2 cm of the vagina developed
- In almost all the patients, the ovarian development is almost normal. And as a result of this, the secondary sexual characteristics like breast development, hair growth, pubic hair growth, and axillary hair growth are all completely normal.
- The karyotyping of almost all the patients is absolutely normal, which is 46XX.
Though the exact prevalence of this disease in India is not known, it is believed to be approximately 1 in 3,000 girls who are known to have MRKH syndrome at birth.
Clinical Features and Symptoms
– What are the primary symptoms of MRKH syndrome?
The first thing that we come to know about a girl who is suspected to have MRKH is basically primary amenorrhea.
That means when other girls start getting periods, these are the girls who do not get their periods. This prompts a little bit of worry, especially in the family members, and especially in the first family, like the mother, and this is one of the most important reasons why these girls are brought to the clinic for an examination.
It is important to typically understand and remember that if a girl does not start getting her menstruation, typically by the age of 13, that means that it warrants an evaluation.
Simultaneously, if we wish to wait, we can wait until the age of fifteen. However, that has to be exercised only if the secondary sexual characteristics, like breast development and axillary and pubic hair growth, have developed very nicely.
In a country like India, the most common cause for having delayed menstruation in such young girls is going to be severe Polycystic Ovary Syndrome (PCOS), and these days, much more commonly, obesity.
What are the different types of MRKH Syndrome?
MRKH syndrome is classified into two types:
- Type 1 (Isolated MRKH): Only the reproductive system is affected
- Type 2 (MRKH with associated anomalies): Includes abnormalities in the kidneys, spine, or heart.
What distinguishes MRKH type 1 from type 2? (MRKH Type 1 vs Type 2)
Typically, based on clinical examination and on doing a per rectal examination; however, it is also very important to understand that in today’s time and age, the majority of the girls would have had an ultrasound or an MRI before they are referred to a unit like ours, because we are a referral unit for MRKH in India.
What associated anomalies are found with MRKH syndrome?
It is prudent to evaluate all these girls for associated abnormalities, especially of the kidney and the entire urinary system.
Absent a kidney or the presence of a kidney at an abnormal location are both very commonly associated features in this syndrome. Some of the girls can also be coming to us with spinal deformity, typically scoliosis, and some of these girls can also have associated cardiac anomalies.
Since we operate on a lot of these girls, we often find in many situations that the kidney is present in the pelvis. This is typically called a pelvic kidney, and as a result, one has to be extremely careful while doing the surgery because of the abnormal position and location of the kidney in the pelvis.

Get Expert Guidance from Dr. Jay Mehta—Müllerian Anomaly Specialist in India
MRKH Syndrome Causes & Genetics
– What are the known causes of MRKH syndrome?
The majority of the time, it is a sporadic event, despite having an absolutely normal genotype.
– Is MRKH syndrome genetic or inherited?
There is no specific genetic link to this condition.
– What genes have been linked to MRKH syndrome?
Yes, certain new genes and their associated abnormalities have been touted as one of the presenting factors that can cause an absent vagina or MRKH syndrome.
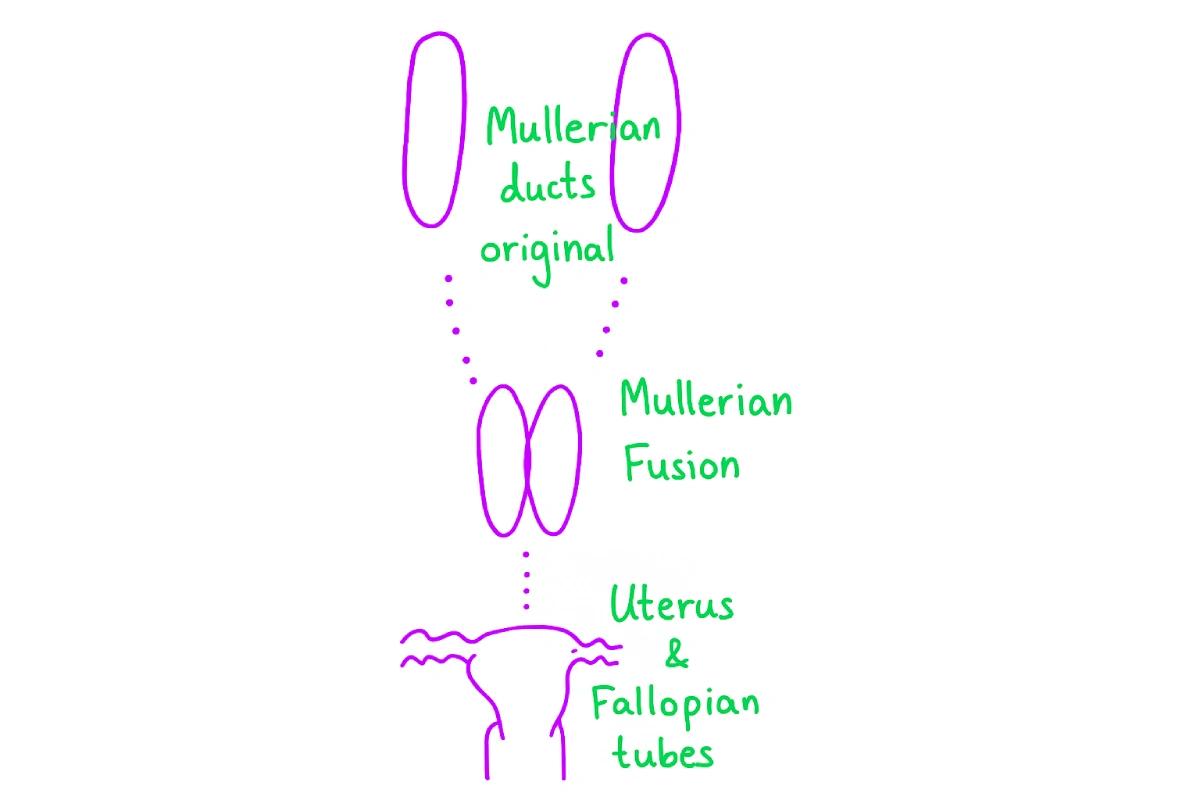
– What embryologic processes are disrupted in MRKH?
The development of the female reproductive system is pretty simple; the uterus and fallopian tubes are developed from the fusion of the Müllerian ducts, which would normally descend downwards. The lower one-third of the vagina develops from the cloacal plate.
Whenever there is a defect in the Müllerian system, it can lead to a situation where both the uterus and the vagina develop abnormally. This is exactly what happens in this condition.
Diagnosis of MRKH Syndrome
– How is MRKH syndrome diagnosed?
MRKH is suspected when a teenage girl presents with absent periods despite normal puberty. Diagnosis involves:
- Physical examination: Noting vaginal depth and development
- Imaging: Pelvic ultrasound and MRI to assess uterine and vaginal structures, and to check for kidney and skeletal anomalies
- Karyotyping: To confirm normal female chromosomes (46XX)
Early and accurate diagnosis helps plan appropriate management and counseling.
Management and Treatment Options for MRKH Syndrome
– What are the treatment options for individuals with MRKH syndrome?
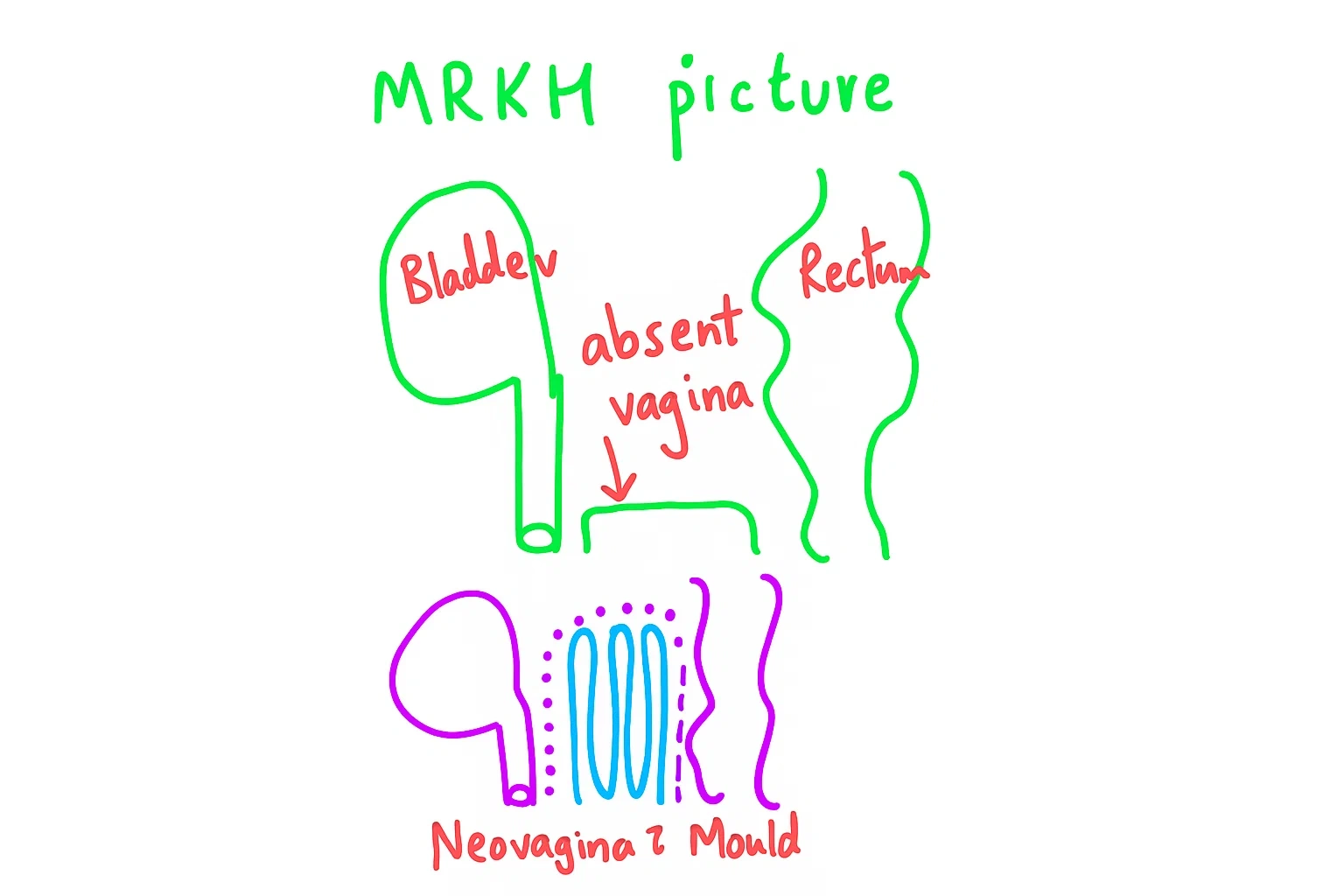
One has to understand that MRKH is an anatomical condition. As a result, if this is to be treated, there is going to be no form of medical management available for this disease. The only effective way to treat this condition is through surgery.
To recreate the absent vagina, we need to understand that the natural vagina is normally formed as a muscular structure.
However, an artificially created vagina is simply going to be a space created by us, either with the help of a laparoscopic or robotic surgery, and the biggest advantage is that it allows us to have sexual function.
One of the most traditional therapies in this context was to use serial vaginal dilation (non-surgical treatment), and that is something that has now been completely outdated and replaced by modern surgical techniques.
The other traditional technique was to use skin grafting, which was predominantly done by plastic surgeons, and it has now been described as a technique that should not be considered in the management of this disease in order to form a new vaginal tract because it can lead to extremely uncomfortable sexual intercourse and a very unhealthy vagina.
For young girls with MRKH, the standard treatment today is minimally invasive surgery, offering better outcomes and faster recovery.
In most cases, surgeons usually create a new vagina (neovagina) in the natural space between the vaginal plate, which is non-functional, and the rectum.
As a referral unit for MRKH across India, we have performed the maximum number of laparoscopic neovaginal reconstructions, as well as redo vaginal reconstructions, for people who have previously attempted a laparoscopic surgery without the available adequate expertise.
Our prime target here is to form an adequate vaginal length of approximately eleven centimeters and ensure a well-formed, functional vaginal apex.
Forming an excellent vagina at the apex with a minimum breadth of approximately four centimeters is extremely important because, no matter how hard we try, there could be some amount of contraction that can occur in this new tract, which has been formed at the end of the procedure.
The vagina is then maintained patent with the help of a Ryles tube mold. The tube is to be maintained in the vagina for at least 6 to 9 months following the surgery. It is an extremely simple technique to form the vaginal tube like this with the help of a Ryles tube.
Most of the girls learn it at the end of the discharge process from the hospital, and more than 99% of them end up doing it, forming it on their own, and placing it in the vagina on their own.
The great advantage of doing this is that it is extremely flexible.
– Why Is Early Surgery Recommended?
Early surgical intervention ensures better healing and outcomes. Unfortunately, in India, many patients undergo inappropriate treatments due to a lack of expertise. It’s crucial to consult a specialist with experience in MRKH surgeries.
– Can people with MRKH have biological children?
Almost all girls with MRKH can have their own biological child. This is because their ovaries are healthy and functional, which means we can retrieve their eggs. However, since the uterus is absent or underdeveloped, pregnancy cannot occur naturally.
In such cases, Assisted Reproductive Technologies (ART)—especially in vitro fertilization (IVF) combined with surrogacy—make it possible to have a biological child. In India, altruistic surrogacy is legally permitted and commonly practiced, giving these young women a safe and reliable path to parenthood.
IVF Involves
- Ovarian stimulation and egg retrieval under ultrasound guidance
- Fertilization with the partner’s sperm in the lab
- Embryo transfer to a surrogate’s uterus to carry the pregnancy
The success rates are comparable to those in women without MRKH.
Mental Health and Social Impact
MRKH can significantly affect psychological well-being:
- Inability to engage in sexual activity may lead to emotional distress
- Social and cultural pressures, particularly regarding marriage in India
Early counseling and proper surgical intervention can significantly improve quality of life
Key Takeaways
- MRKH syndrome is rare but manageable with modern surgical techniques.
- Early diagnosis ensures better outcomes in vaginal reconstruction.
- Fertility remains achievable with IVF and surrogacy.
- Expert counseling and referral to specialized units are crucial.
If you or your loved one is affected by MRKH syndrome, don’t wait. Early evaluation and expert care make all the difference. Book a consultation with Dr. Jay Mehta, a leading specialist in MRKH treatment and reproductive surgery, and take the first step toward improved quality of life and reproductive health.
FAQs About MRKH Syndrome
– What is the first sign of MRKH syndrome?
The earliest sign of MRKH syndrome is the absence of menstruation (primary amenorrhea), where a girl does not start her periods by the expected age despite normal growth and development.
– Can MRKH syndrome be cured?
There is no permanent cure for MRKH syndrome because it is a developmental condition present from birth. Still, minimally invasive surgery can successfully recreate a vagina, which helps restore sexual function and improves overall confidence and well-being.
– Can MRKH patients have sexual activity?
Yes, MRKH patients can have sexual activity after neovaginal reconstruction surgery.
– Is MRKH syndrome genetic?
Most cases of MRKH syndrome occur sporadically, meaning they are not inherited. However, research suggests that certain genetic factors may play a role in some patients.
– When should MRKH be diagnosed?
If menstruation hasn’t started by age 13–15, especially with normal secondary sexual development, evaluation is warranted.
– Can MRKH patients carry their own pregnancy?
No, women with MRKH cannot carry a pregnancy themselves because the uterus is absent or underdeveloped. Currently, uterus transplantation is still experimental, so pregnancy requires the use of a surrogate.
– What is the best treatment for MRKH syndrome?
The best treatment for MRKH syndrome is minimally invasive surgery, most commonly laparoscopic neovagina creation, which safely and effectively creates a functional vagina.
– Are kidneys always affected in MRKH?
No, kidneys are not always affected in MRKH syndrome, but kidney malformations are fairly common. That’s why a thorough evaluation of the urinary system is recommended
Dr Jay Mehta
Scientific Director & IVF Specialist with 10+ years of experience
CALL US 24/7 FOR ANY HELP
GET IN TOUCH ON


