Uterine Prolapse: How it Affects Women at Different Life Stages
UPDATED ON 18 OCT. 2023
Uterine prolapse and its impact on women in various stages of life. As a leading expert in gynaecology with years of experience, we understand your concerns and questions about this condition.
Our goal is to provide you with valuable information that empowers you to make informed decisions about your health.
AUTHOR
Dr Jay Mehta
Scientific Director & IVF Specialist with 10+ years of experience
CONDITION
GET IN TOUCH ON
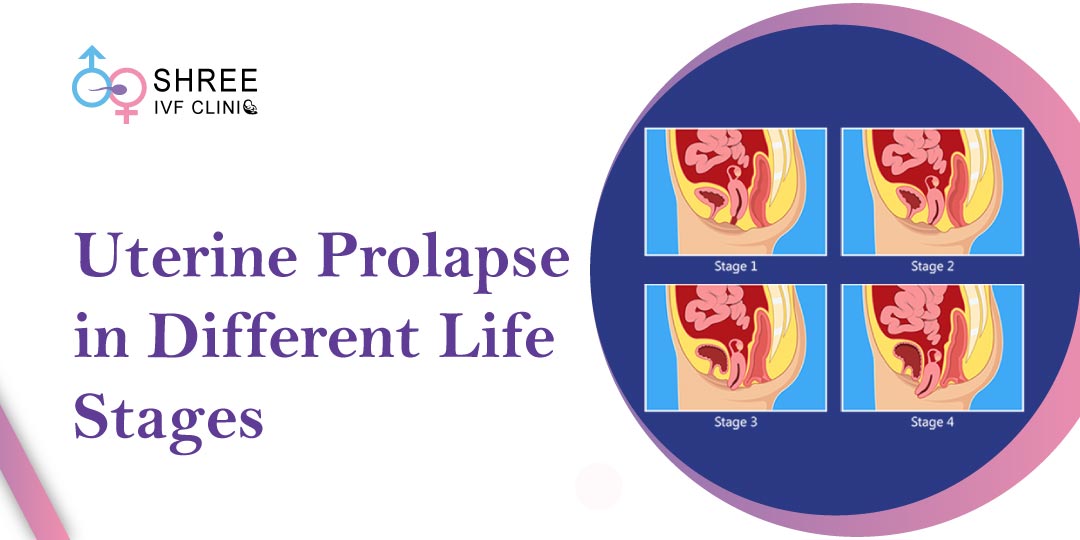
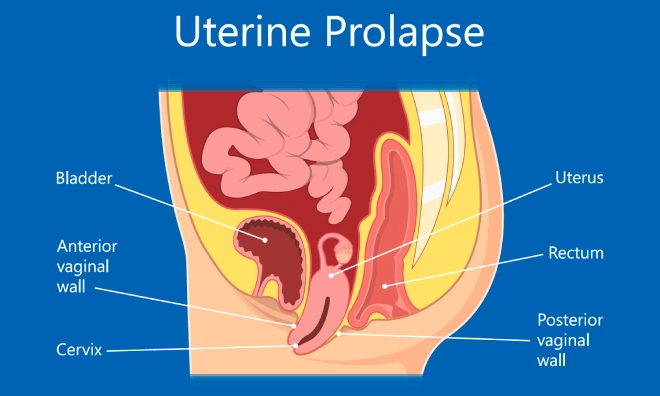
What is Uterine Prolapse?
Uterine prolapse occurs when the muscles and ligaments supporting the uterus weaken, causing it to descend into the vaginal canal. This can result from age, genetic predisposition, repeated childbirth, obesity, chronic coughing, and hormonal changes.
Understanding the anatomical factors involved in uterine prolapse is crucial for comprehending why this condition develops. We will explore the intricate structures of the pelvic floor and how they contribute to uterine prolapse.
Additionally, we will discuss the different types of uterine prolapse, including anterior, posterior, and complete prolapse, and their specific characteristics.
Risk Factors and Causes

Certain factors increase the likelihood of developing uterine prolapse. These include multiple pregnancies, vaginal deliveries, giving birth to a large baby, obesity, heavy lifting, chronic conditions like constipation and respiratory problems, and hormonal changes during menopause.
While these factors do not guarantee uterine prolapse, they contribute to weakening the pelvic floor muscles and ligaments, making it more susceptible. We will discuss each risk factor in detail and explain how it impacts the development of uterine prolapse. Additionally, we will explore the role of connective tissue disorders and hormonal imbalances in increasing the risk of prolapse.
also Read: What Are Prolapsed Uterus Treatment at Home?
Uterine Prolapse During Reproductive Years
If you are in your reproductive years, uterine prolapse may present unique challenges. Symptoms can include a sensation of heaviness or pressure in the pelvis, difficulty emptying the bladder, recurrent urinary tract infections, and discomfort during sexual intercourse.
We’ll explore how uterine prolapse during this stage can be managed effectively, providing you with practical tips and guidance.
We will discuss non-surgical treatment options such as pelvic floor exercises, lifestyle modifications, pessary use, and hormonal therapies to alleviate symptoms and improve quality of life.
Furthermore, we will delve into the emotional and psychological impact of uterine prolapse during reproductive years and provide strategies for coping with these challenges.
Uterine Prolapse Post-Menopause
After menopause, hormonal changes can impact the strength and elasticity of pelvic tissues. This can lead to a different set of symptoms, such as vaginal dryness, urinary incontinence, and changes in sexual function.
We’ll discuss treatment options for post-menopausal women that cater specifically to their needs, allowing you to regain control over your health and well-being.
In addition to non-surgical approaches, we will also explore surgical interventions like uterine suspension procedures and hysterectomy for those with severe symptoms.
We will discuss the potential benefits and risks associated with hormone replacement therapy (HRT) and other medications in managing post-menopausal symptoms.
Uterine Prolapse After Childbirth
Childbirth can significantly affect the likelihood of developing uterine prolapse. The pressure exerted on the pelvic floor during labor, especially in cases of prolonged or difficult deliveries, can weaken the supporting structures of the uterus.
We will provide valuable insights into preventive measures and treatment options for women who have recently given birth, ensuring a smooth recovery and reducing the risk of prolapse.
We will discuss the importance of postpartum pelvic floor rehabilitation and the benefits of specific exercises and techniques to strengthen the pelvic floor muscles.
Additionally, we will address the emotional aspects of dealing with uterine prolapse after childbirth and provide support strategies for new mothers.

4,790+
379K+
” Every individual and couple’s journey is unique, and
finding the right solutions tailored to their specific
circumstances can make all the difference “
Diagnosis and Treatment
Diagnosing uterine prolapse involves a comprehensive medical evaluation, including a physical examination and possibly imaging tests. Our expert gynecologists will guide you through this process and discuss various treatment options tailored to your individual circumstances.
From non-invasive approaches like lifestyle modifications, pelvic floor exercises, and pessary use to surgical interventions, such as uterine suspension procedures and hysterectomy, we will explain the choices available to help you make informed decisions about your treatment plan. We will also discuss the potential risks and benefits associated with each treatment option
Diagnosing uterine prolapse involves a comprehensive medical evaluation, including a physical examination and possibly imaging tests.
Our expert gynecologists will guide you through this process and discuss various treatment options tailored to your individual circumstances.
From non-invasive approaches like lifestyle modifications, pelvic floor exercises, and pessary use to surgical interventions, such as uterine suspension procedures and hysterectomy, we will explain the choices available to help you make informed decisions about your treatment plan.
We will also discuss the potential risks and benefits associated with each treatment option.
In terms of non-surgical treatments, pelvic floor exercises play a crucial role in strengthening the pelvic floor muscles and improving support for the uterus. These exercises, known as Kegels, involve contracting and relaxing the pelvic floor muscles to enhance their tone and function.
Lifestyle modifications, such as maintaining a healthy weight, avoiding heavy lifting, and managing chronic conditions like constipation and respiratory problems, can also alleviate symptoms and prevent further progression of uterine prolapse.
Additionally, the use of a pessary, a device inserted into the vagina to provide support to the uterus, can be an effective non-surgical option for managing uterine prolapse.
However, in some cases, surgical intervention may be necessary. Uterine suspension procedures, such as uterosacral ligament suspension, involve repositioning and supporting the uterus using mesh or sutures.
These procedures aim to restore the normal anatomical position of the uterus and enhance its stability. In more severe cases or when other treatments have been unsuccessful, a hysterectomy may be recommended.
A hysterectomy involves the removal of the uterus and can provide long-term relief from uterine prolapse. However, it is important to carefully consider the potential impact on future fertility and hormonal balance before opting for this surgical procedure.
Lifestyle and Self-Care Tips
In addition to medical interventions, specific lifestyle changes can be beneficial in managing uterine prolapse.
We will provide practical self-care tips, including maintaining a healthy weight, avoiding heavy lifting, practising good posture, incorporating regular physical activity, and managing chronic conditions like constipation and respiratory problems.
These measures will help strengthen the pelvic floor muscles and reduce the risk of prolapse progression. We will also discuss the importance of regular follow-up visits with your gynaecologist to monitor your condition and make necessary adjustments to your treatment plan.
Reclaim Your Comfort! Trust Shree IVF Hospital for Expert Pelvic Organ Prolapse Treatment. Contact us now
Seeking Professional Help
If you suspect or experience symptoms of uterine prolapse, it is crucial to seek professional help from our experienced gynecologists.
They have the expertise and knowledge to provide a comprehensive evaluation, accurate diagnosis, and personalized treatment options tailored to your specific needs. Our team at Shree IVF clinic is dedicated to providing compassionate and patient-centered care.
Conclusion
Understanding uterine prolapse at different life stages is crucial for women’s overall health and well-being.
By providing comprehensive information on causes, symptoms, risk factors, and treatment options, we aim to empower you to take control of your health.
Remember, you don’t have to face uterine prolapse alone. Our team of expert gynecologists at Shree IVF clinic is here to support you every step of the way, ensuring you receive the best possible care for this condition.
Take charge of your health today and schedule a consultation with our gynecologists. Together, we can develop an individualized treatment plan that meets your needs and improves your quality of life. Don’t let uterine prolapse hold you back.
With the right support and guidance, you can regain control and live your life to the fullest. Contact us at Shree IVF clinic and let us be your partner in your journey towards optimal pelvic health.
AUTHOR
Dr Jay Mehta
Scientific Director & IVF Specialist with 10+ years of experience
CONDITION
CALL US 24/7 FOR ANY HELP
GET IN TOUCH ON
Share Article on
Recommended Reading
How is a Bleeding Prolapse Treated?
Epithelial, Germ Cell, and Stromal are ovarian cancer types which are classified by their originating cells
Can Pelvic Organ Prolapse Go Away On Its Own?
Uncover the potential for pelvic organ prolapse (POP) to resolve naturally. Explore symptoms, management options, and factors influencing resolution.
Can Pelvic Organ Prolapse be a Sign of Cancer?
Pelvic Organ Prolapse (POP) doesn’t directly cause cancer, but women with this condition are at a higher risk of developing certain cancers like uterine & gallbladder cancers




