From Causes to Risks: Decoding Uterine Prolapse
UPDATED ON 9 OCT. 2023
Maintaining optimal pelvic health is crucial for women’s overall well-being. One condition that affects many women worldwide is uterine prolapse.
This blog post will delve deeper into the causes, risk factors, and prevention strategies associated with uterine prolapse.

AUTHOR
Dr Jay Mehta
Scientific Director & IVF Specialist with 10+ years of experience
CONDITION
GET IN TOUCH ON
What is Uterine Prolapse?
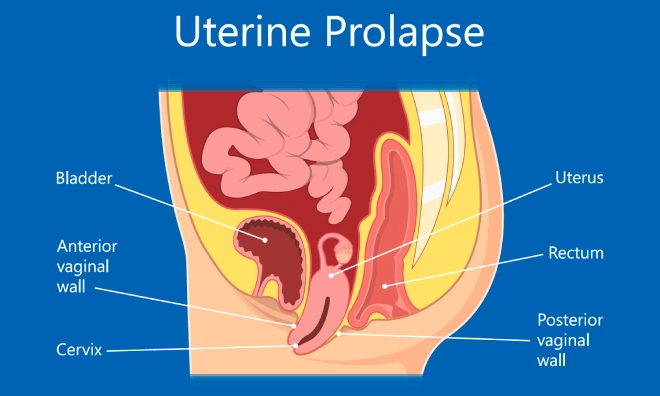
The uterus, a critical reproductive organ, can descend into the vaginal canal due to weakened pelvic floor muscles and ligaments. Uterine prolapse occurs when this descent becomes significant enough to cause discomfort or an evident bulging sensation.
It is vital to grasp the anatomy of the uterus and the various types of uterine prolapse to understand better this condition and its potential impact on women’s lives.
There are different types of uterine prolapse, including:
⇒ First-Degree Prolapse: The uterus descends slightly into the vagina.
⇒ Second-Degree Prolapse: The uterus extends further into the vagina but does not protrude outside.
⇒ Third-Degree Prolapse: The uterus protrudes outside the vagina.
Understanding the severity and classification of uterine prolapse helps determine appropriate treatment options.
Also Read: Uterine Prolapse: How it Affects Women at Different Life Stages
Causes of Uterine Prolapse
Childbirth and pregnancy often contribute to uterine prolapse. The strain placed on the pelvic floor during vaginal delivery, particularly in cases of multiple pregnancies, can weaken the supporting structures.
The intense pressure exerted during labour and delivery stretches and weakens the muscles, ligaments, and tissues holding the uterus.
Hormonal changes also significantly affect uterine prolapse, especially during menopause. Estrogen, a hormone vital for maintaining tissue strength, gradually decreases during menopause, impacting the integrity of the uterine support structures.
This hormonal shift leads to decreased muscle tone and the loss of elasticity in connective tissues, making the uterus more susceptible to prolapse.
In addition to childbirth and hormonal changes, several other factors contribute to uterine prolapse. These include:
⇒ Muscle Weakness: Chronic conditions like obesity, chronic cough, or constipation can weaken the pelvic floor muscles, increasing the risk of prolapse.
⇒ Connective Tissue Damage: Conditions such as Ehlers-Danlos syndrome or Marfan syndrome, which affect the connective tissues, can make women more prone to uterine prolapse.
⇒ Chronic Conditions: Certain chronic health conditions, such as asthma or bronchitis, that cause persistent coughing can strain the pelvic floor muscles and increase the risk of prolapse.
⇒ Lifestyle Factors: Engaging in activities that involve heavy lifting, repetitive straining, or high-impact exercises can put excessive pressure on the pelvic region, leading to muscle weakness and prolapse.
It is crucial to note that every woman’s experience with uterine prolapse is unique, and multiple factors can contribute to its development.
Risk Factors for Uterine Prolapse
Certain factors increase a woman’s vulnerability to uterine prolapse. Understanding these risk factors can help individuals identify their susceptibility to the condition and take necessary precautions. Some common risk factors include:
⇒ Age and Hormonal Changes:
The risk of uterine prolapse increases with age, particularly during and after menopause, when estrogen levels decline, weakening the pelvic floor muscles and tissues.
⇒ Genetic Predisposition:
Some women may have an inherent weakness in their pelvic floor muscles or connective tissues due to genetic factors, making them more prone to uterine prolapse.
⇒ Ethnicity:
Studies suggest that certain ethnicities, such as African, Hispanic, and Caucasian, have a higher prevalence of uterine prolapse. The reasons for these differences are still being researched.
⇒ Occupational Risks:
Jobs that involve prolonged periods of standing or heavy lifting, such as nursing or manual labour, can strain the pelvic floor muscles, increasing the risk of prolapse.
It is important to note that having one or more risk factors does not necessarily mean a woman will develop uterine prolapse. Each person’s experience may vary, and understanding the risk factors helps take appropriate preventive measures.
Also Read: Can Uterus Prolapse Lead to Miscarriage?

4,790+
379K+
” Every individual and couple’s journey is unique, and
finding the right solutions tailored to their specific
circumstances can make all the difference “
Prevention Strategies
While uterine prolapse cannot always be entirely prevented, specific strategies can help minimize the risk and maintain optimal pelvic health. Here are some effective prevention strategies:
⇒ Pelvic Floor Exercises: Regularly performing pelvic floor exercises, such as Kegels, can strengthen the muscles that support the uterus. These exercises involve contracting and relaxing the pelvic floor muscles, promoting their tone and endurance.
⇒ Maintain a Healthy Weight: Excess weight puts added pressure on the pelvic floor muscles, increasing the risk of prolapse. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce this pressure and promote pelvic health.
⇒ Avoid Heavy Lifting: Engaging in heavy lifting activities can strain the pelvic floor muscles and increase the risk of uterine prolapse. When lifting heavy objects, ensure proper technique and use your legs instead of relying solely on your back and pelvic area.
⇒ Manage Chronic Conditions: If you have chronic conditions such as asthma or bronchitis that cause persistent coughing, seek appropriate medical management to minimise the strain on your pelvic floor muscles.
⇒ Practice Good Toilet Habits: Avoid straining during bowel movements by maintaining a healthy fibre-rich diet and staying hydrated. Straining can weaken the pelvic floor muscles over time, increasing the risk of prolapse.
⇒ Regular Medical Checkups: Routine checkups with gynaecologist are essential for early detection and intervention. A gynaecologist can assess your pelvic health and address any concerns or symptoms related to uterine prolapse. Early detection allows prompt treatment and a better chance of managing the condition effectively.
Conclusion
Understanding uterine prolapse empowers women to prioritise their pelvic health. By comprehending the causes, risk factors, and prevention strategies associated with this condition, women can take proactive steps to prevent it and seek appropriate medical guidance when needed.
Remember, your health matters, and staying informed and advocating for your well-being is essential. With a focus on prevention strategies, regular pelvic floor exercises, and early intervention through medical checkups, we can work together to support women’s pelvic health and ensure a better quality of life.
At Shree IVF Clinic, we are dedicated to providing patient-centred care and support. If you have any concerns or questions about uterine prolapse treatment or any other aspect of women’s health, our team of experienced gynaecologists is here to guide you. Take charge of your pelvic health and prioritise your well-being today.
AUTHOR
Dr Jay Mehta
Scientific Director & IVF Specialist with 10+ years of experience
CONDITION
CALL US 24/7 FOR ANY HELP
GET IN TOUCH ON
Share Article on
Recommended Reading
How is a Bleeding Prolapse Treated?
Epithelial, Germ Cell, and Stromal are ovarian cancer types which are classified by their originating cells
Can Pelvic Organ Prolapse Go Away On Its Own?
Uncover the potential for pelvic organ prolapse (POP) to resolve naturally. Explore symptoms, management options, and factors influencing resolution.
Can Pelvic Organ Prolapse be a Sign of Cancer?
Pelvic Organ Prolapse (POP) doesn’t directly cause cancer, but women with this condition are at a higher risk of developing certain cancers like uterine & gallbladder cancers




